Minimally invasive cervical fusion surgery, sometimes known as anterior cervical discectomy and fusion (ACDF), removes a herniated or degenerative disc in the neck. But what’s interesting is, the disc is removed through an incision in the throat, and the bones above and below the disc are fused together with a graft.
You might need same-day “awake” ACDF surgery if physical therapy, medications, or lifestyle changes don’t remedy your debilitating upper-back or neck pain. The nice part is, the patient usually goes home almost immediately after the procedure.
What’s even better: If you’re used to working full-time, you can be assured you’ll most likely return to work relatively soon under the circumstances after undergoing surgery, according to some positive research on post-operative patients. It will depend on your type of job, but many patients are reporting great results.
So, what is this surgery all about?
Minimally Invasive Cervical Fusion: What is It?
From the neck to the low back, discectomy literally means “cutting out the disc.” During a minimally invasive cervical fusion, this is accomplished by reaching the damaged disc through the throat. The disc and bony vertebrae are exposed when you move the neck muscles, trachea, and esophagus aside.
It’s easier to access the disc from the front of the neck than from the back because it can’t be disturbed by the spinal cord or spinal nerves. The number of discs removed will depend on your symptoms.
The space between the bony vertebrae is empty after the disc is removed. A spacer-bone graft fills the gap between the vertebrae to prevent them from collapsing. The graft connects two vertebrae to create a spinal fusion. Using metal plates and screws, the bone graft and vertebrae are fixed in place.
As soon as the surgery is over, the body starts healing itself and new bone cells grow around the graft. Usually the bone graft takes 3 – 6 months to join the two vertebrae together. It’s like reinforced concrete, where the instrumentation and fusion work in harmony.
How is Minimally Invasive Cervical Fusion Performed?
Surgery usually it takes 1 – 3 hours depending on the patient. It truly is a miracle:
Anesthesia will be administered while you’re lying on your back. You’ll get a clean and prepped neck once you’re asleep. Your hip area is also prepped if you’re having a fusion where your own bone is used; however, your hip incision isn’t needed if a donor bone is used.
The second step of a minimally invasive cervical fusion is to make the incision. On the right or left side of your neck, you’ll have a two-inch skin incision. The surgeon moves muscles in your neck and retracts the trachea, esophagus, and arteries to make a tunnel to the spine. The surgeon will be able to see the bony vertebrae and discs. Muscles supporting the front of the spine are also lifted and held aside.
Next, the surgeon finds out where the disc is damaged. An X-ray called a fluoroscope helps the surgeon locate the affected vertebra and disc with a thin needle. With a special retractor, the vertebrae above and below the damaged disc are spread apart.
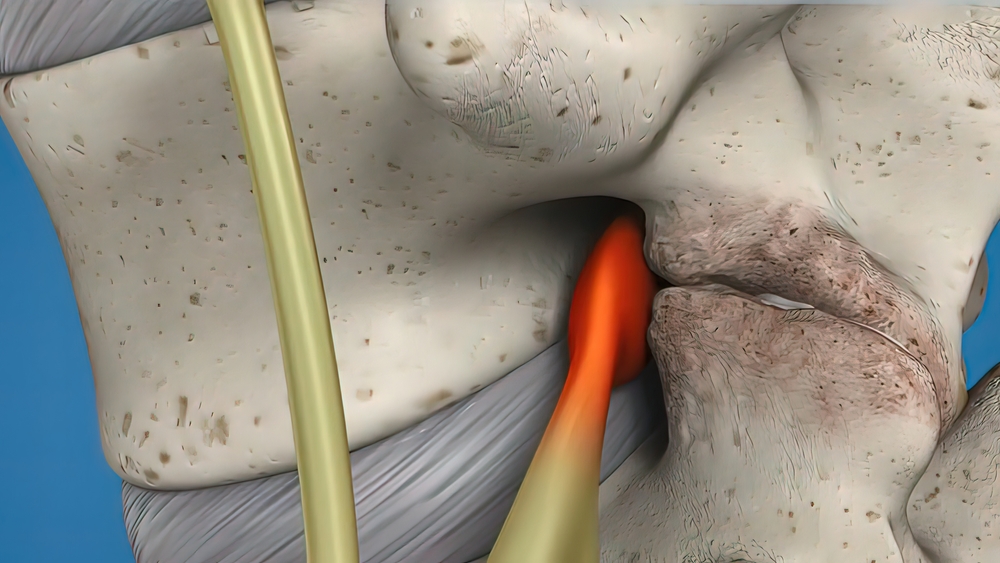
Now it’s time to remove the disc. A cut is made on the disc’s outer wall. About two-thirds of your disc is removed with small grasping tools, and the rest is removed through a surgical microscope. To get to the spinal canal, the surgeon must cut the ligament behind the vertebrae. Spinal nerves are relieved of any disc material pressing on them. This decompresses the nerve, and nerve root pressure is relieved by removing bone spurs as well. Drilling enlarges the passageway where the spinal nerve exits so nerves can exit the spinal canal more easily.
Lastly, a bone-graft fusion is prepared. The outer layer of bone is removed with a drill. You and your surgeon will choose bone graft material for this “bed” — and usually the patient’s hip is a good candidate. An incision is made over your own hipbone crest, and once the hard outer layer is cut, the inner layer is accessed with a chisel. The surgeon shapes the bone graft and places it between the neck vertebrae. A cadaver bone graft is used in other cases depending on your surgery plans. Afterward, the graft is tapped into place. During fusion, a metal plate is usually screwed into the vertebrae to reinforce the bone graft.
Finally, the incision is closed using special sterilized strips or medical-surgery glue. The miracle is completed safely and securely.
Are You a Candidate for Surgery?
If your situation and pain do not improve as you try figuring out what’s wrong with your neck or back, you might find you have a herniated or degenerative disc, significant weakening in your hand or arm, or arm pain that’s worse than neck pain. Usually an MRI, CT scan, or a myelogram (diagnostic imaging test) can tell you if you’re a good candidate for “awake” minimally invasive cervical fusion surgery.
This type of surgery can be perfect for remedying a disc that’s bulging or herniated. A weak spot in the surrounding wall can cause the gel-like material inside the disc to bulge or rupture. Nerves are irritated and swollen when this material squeezes out.
In other instances, someone might have degenerative disc disease. Bone spurs form when discs wear out, causing inflammation in the facet joints. Disks lose their flexibility and cushioning properties as they dry out and shrink. Essentially, there’s less room within the discs. Disc herniation or canal stenosis can result from these changes.
If you happen to undergo surgery, you’ll want to prepare a healthy and balanced meal plan to help your body recover much faster post-procedure.
Consider Options and Weigh the Benefits
Not every pain problem needs surgery as a fix. Non-surgical treatment heals most herniated discs. After six weeks of conservative therapy, usually only a small percentage of people with herniated discs have enough pain to consider and warrant surgery.
Still, a minimally invasive cervical fusion just might be what you need. Surgery may be recommended by your doctor, but only you can decide if it’s right for you. Don’t make a decision until you’ve considered all the benefits.
Awake Spinal Fusion is here to educate you on the basics of your spine, back pain, “awake” spinal and neck surgery, minimally invasive surgery options, and much more.






